Pellucid Marginal Degeneration is Keratoconus
- August 15, 2022
What is Pellucid Marginal Degeneration?
So, your eye doctor diagnosed you with pellucid marginal degeneration (PMD). PMD is an eye disease where the front clear dome of the eye, the cornea, is distorted and blurs vision. But how is PMD different from keratoconus, where the cornea is also distorted? If you are confused, you are not alone. Even some general eye doctors are confused!
Pellucid Marginal Degeneration
Researchers and eye doctors used to believe that PMD was a separate disease from keratoconus. Hallmarks of PMD supposedly included a “crab-claw” or “butterfly” patterned corneal topography, a diagnostic measurement which generates a color map representing the light-bending power of the cornea. Another claimed characteristic of PMD was that the disease
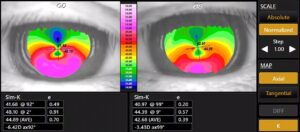
Figure 1. “Crab-claw” or “butterfly” pattern corneal topography previously thought to indicate pellucid marginal degeneration.
would begin in the third-to-fourth decade of life. By comparison, with most keratoconus, onset is during the adolescent years.
The Keratoconus Global Consensus
Today, most experts believe that PMD and keratoconus are actually the same thing, although PMD and classic keratoconus exhibit different patterns of distortion. With PMD, the corneal distortion involves a larger bulge on the bottom. Indeed, the World Health Organization does not assign a separate diagnostic code, i.e., an IDC-10 code or 10th revision of the International Statistical Classification of Diseases and Related Health Problems. Instead, PMD is just coded as keratoconus.
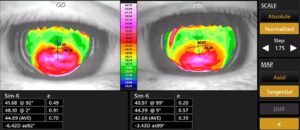
Figure 2. Same topography as Figure 1 but under a tangential view.
Two factors previously confused eye doctors into believing that PMD and keratoconus were separate eye conditions. First, the classic “crab-claw” or “butterfly” topography pattern attributed to PMD (Figure 1) was just due to the way the topographical map was viewed. A topography can be viewed as an “axial map” which smooths out data points, or as a “tangential” map which provides a more point-to-point assessment of light bending power. Reprocessing an axial topography to tangential view generally uncovers a classic keratoconus pattern for most alleged cases of PMD (Figure 2). Second, PMD supposedly had a later onset in life. But in fact, PMD is often diagnosed later because it tends to impact vision less. Many eye doctors and patients incorrectly assumed that the time of diagnosis was also the time of onset. Since many patients with PMD achieve good vision with eyeglasses with the bulk of the corneal distortion decentered downward out of the line of sight, PMD would often get diagnosed later because vision symptoms often are more subtle. In other words, most patients with PMD likely had onset of their corneal distortion in the adolescent years despite diagnosis coming much later due to mild symptoms.
The fact that some patients have a PMD-type topography in one eye and a more classic keratoconus topography in their other eye, also supports that these are the same disease entity.
PMD: A Variant of Keratoconus
PMD is the same thing as keratoconus, just a subclass of it. If your doctor told you that you have PMD, you likely get decent vision with updated eyeglasses and received diagnosis later in life compared to others with keratoconus. The treatment to restore vision is the same if you have PMD or classic keratoconus: specialty contact lenses with a rigid surface are the gold standard for visual rehabilitation. These days, scleral contact lenses are a common and effective treatment for keratoconus, including if your eye doctor diagnosed PMD.
To learn more about your keratoconus, call ReVision Optometry today to schedule your examination at 619.299.6064 or request an appointment online. During your examination, you will learn about your candidacy for scleral lenses, including an estimate of out-of-pocket costs.
